Caring for my husband profoundly changed my life. I was a wife, mother, and retired registered nurse, then became my husband Rick's primary caregiver as well. I knew Rick well. From the way he slightly lowered his head and tilted it to one side, I could tell he had had enough for the day. He faced never ending challenges, and was often exhausted.
When did you meet your husband?
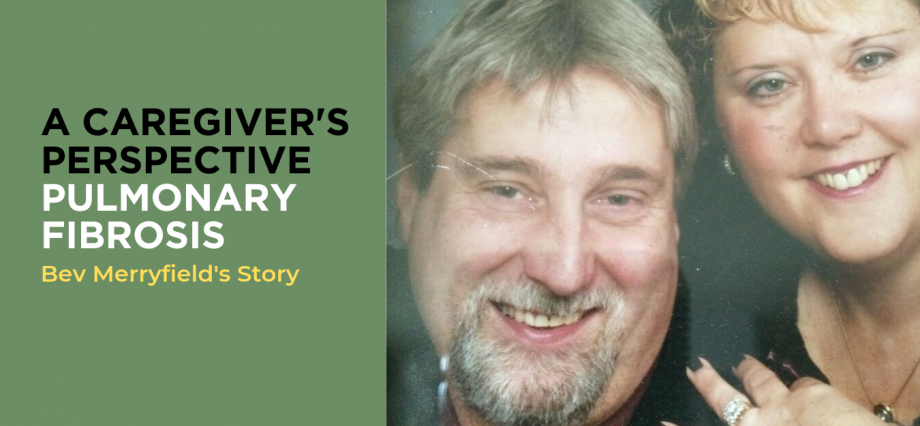
Rick and I were high school sweethearts. After I graduated from nursing school in 1980, we married and started a family – two girls and a boy. Rick was self-employed in the construction industry while I enjoyed a career as a registered nurse. I worked in Victoria for the Vancouver Island Health Authority, serving in many different capacities from point of care nursing to leadership roles, retiring last year after 38 years of service.
By 2011, our children had all left home enabling Rick and I to live travel. We had a few great trips when Rick contracted pneumonia twice in a few short months, leading his GP to do further testing and ultimately referring him to a respirologist.
What did you do when Rick was diagnosed with a lung condition?
The first thing we did was travel more when Rick was diagnosed with PF (Pulmonary Fibrosis), a rare and progressive lung disease that causes scarring of the alveoli and interstitial tissues of the lungs. What surprised us was Rick had never smoked and was asymptomatic prior to his diagnosis, so lung disease was not something we were prepared to hear.
Rick was a burly guy so he faired very well with treatment the first year. But into his second year, life became increasingly more difficult with the onset of fatigue, laboured coughing, and shortness of breath. He compensated by working part-time and eventually was forced to stop working completely. He managed to live with PF for five years before it progressed to a point where he needed to be put on the lung transplant list.
What challenges did Rick face while receiving a lung transplant?
On January 23, 2017 at Vancouver General Hospital (VGH), Rick received a double lung transplant as well as five coronary bypass graphs that dealt with plaque blockages as a result of chronic diseases (diabetes) and medications.
After a bumpy few days adjusting to his new lungs, he awoke asking for glasses and a book to read. However, the next day he became drowsier and was once again unconscious by the evening. A stroke was a real possibility and the ICU team leapt into action, keeping us in the loop with each test and plan of care, which often changed one hour to the next. After many days of tests, specialists, and a host of medications, the doctors discovered an extremely rare bug in his lungs. The rare bug caused a cascade of complications and medical challenges bringing many different specialists and expertise to his side as he fought for his life.
Why did Rick’s care team call him the miracle man?
Because Rick kept beating the odds… I believe the care team saw Rick as not just a patient, but more as a miracle man with a spirit that wouldn't give up! He slowly regained consciousness and was able to move his arms and legs very weakly again. He spent another month in the Respiratory Unit at VGH where he regained strength, learned to breathe on his own, and eat!
On April 5th, 2017 (our 37th wedding anniversary) Rick was transferred to Vancouver's GF Strong Rehabilitation Centre where we believed his road to recovery would be fulfilled. We knew it would take time and was going to be hard work, but that is who Rick was!
Rick being fiercely independent and perhaps a little stubborn, it was important to both of us for him to do as much of his own care as possible. I was able to provide him with the time, direction, support, and encouragement to do for himself while looking for subtle hints that he was getting tired or frustrated – and I could tell not because of my nursing experience, but because of the lifetime partnership we shared. The hospital staff was always there for us, even while they were busy no matter the time of day or night.
Were you part of the care team, participating in discussions/decisions?
When Rick was in the ward, it was hard not being part of rounds with the care team. The doctor or staff member often came to talk to us after the rounds. However, we didn't feel like we had a voice in the moment of discussions/decisions with the team. Consequently, I had to hover around, waiting for an update or to have questions answered. I didn't want to leave in case I missed the doctor. This contrasted with our experience after Rick came out of surgery and was in ICU, where we valued meeting and discussing his care together with the medical team. When he was the sickest, hanging onto life, that is when I felt we were part of the team.
Sadly, one of the hard truths is that not every one is going to win their fight.
While in GF Strong, Rick got really sick again. First his blood work was abnormal, and then he got flu like symptoms. We knew something was going on. He was weak and slept most of the time. While he never complained, he did say he was getting tired of feeling positive one moment only to feel discouraged the next. A few days later he became unconscious and went into septic shock. He never came out of it.
On May 1st, 2017, Rick died of post-transplant Lymph-proliferative disorder (Lymphoma). Rick's autopsy report was devastating – the lymphoma was so widespread throughout his organs there was no chance he could have beat it. It was heartbreaking and didn't seem fair, but I am so grateful I was able to spend each and every day by his side.
Do you think the role of patient caregiver would benefit from greater definition?
Yes. In my experience the caregiver role and its relationship within the patient's care team remains vague and varied depending on where you are in the journey. At home or in the community, it seems more open but in some parts of the hospital you feel “left out” or perhaps not fully heard. I think one improvement may be to determine what style of communication and how much information is most effective for a given patient and caregiver from the onset.
Do you think patients and caregivers need more support and guidance about the logistics involved in situations like Rick’s?
When we got the call to say they were ready to perform Rick’s lung transplant, we had to leave Victoria and move to Vancouver. Rick spent 95 days in hospital in Vancouver over the course of his illness. And as supportive as the hospital was from a medical standpoint, there was little help with logistics like accommodations, etc.
I was thankful Rick and I had started saving money early. We saved so we could hire people to help out at home in Victoria to support Rick’s mother who lived with us, and so we could afford accommodation in Vancouver. And, I’m so grateful for friends who jumped in and booked a hotel close to VGH and helped me find a place to stay. Our three grown children, six grandchildren, and other family members were stars in their own right too, looking after one another and great grandma while Rick and I were staying in Vancouver.
Is there any other special help you received?
I know I could not have managed without the support of my best friend. She took me away after Rick was gone, and that short time away allowed me to fall apart and then pull myself back together again. We shared a lot of tears and memories. Coming home, I had to face life in a new way, a way I had never planned. Six weeks later I returned to work, back to a job I loved but with a heavy heart. I'm so grateful to everyone at work for being so understanding and supportive.
Rick was part of a large business community, volunteer network, and plethora of sport associations. From the time he was diagnosed with PF, we created strong lines of communications so that everybody who cared about him was up to date with how he was doing. And we still communicate now.
What has helped you since that time?
As a family, we began to create new traditions in to honour Rick. For example, one of the things I do is to make sure he has a present for me on my birthday and one for me under the Christmas tree, thoughtfully chosen and wrapped. I thank Rick for these presents as if he was sitting right beside me. They are a reminder that even though he is no longer with us physically, spiritually and emotionally he is still very much part of our family.
How do you feel now as you look back on Rick’s lung journey?
I remember saying to myself, “Just get through today, one step at a time, one test at a time.” I wrote in a journal to help keep my head above water, to help remember what was being said and to keep track of who was who in the zoo. I wrote because I wanted Rick to read my journal, to understand how much he went through, and just how much of a miracle man he truly was.
How do you reflect on Rick and his journey now?
Rick was a courageous human being who did not let his illness define him. If I could talk to Rick right now, I would thank him for being an extraordinary husband, father, and papa – and for allowing me the privilege of being his caregiver – doing so was the hardest but most wonderful thing I’ve ever done in my life. Being by Rick’s side on this journey provided me with the finest examples of courage, humility, and humanity I’ve ever witnessed. It profoundly changed my life, and I am grateful beyond measure.